Your days in the sun can affect your eyes and the rest of your body. Protecting your vision and ocular health can reduce your risk of certain eye diseases and conditions as you age, including cataracts and eye cancers. Our eye doctors in Kansas City and St. Joseph hope you enjoy a fun summer. Remember to take care of your eyes using these tips, and schedule annual eye exams to diagnose and treat vision problems early.
1. Sunglasses with “100% UV Protection” for the Whole Family
Babies, children and adults of all ages need to protect their eyes outdoors, including on hazy or cloudy days. UV-protective sunglasses are an essential part of eye care for the whole family, and they should wear these frames year-round. Wrap-around sunglasses are best because they cover your entire visual field, and wide-brimmed hats can help reduce UV exposure.
It can take decades for UV rays to harm your eyes, but you increase your risk of cataracts and eye cancers each time you forget your sunglasses at home. Harmful UV rays can cause “sunburn of the eye” or photokeratitis. This condition happens when UV exposure burns the eye’s surface, leading to temporary vision loss, redness, blurry vision and eye pain. Sunlight that reflects off of water, sand, ice and snow can cause photokeratitis and snow blindness (a form of photokeratitis). Surfers, skiers, farmers and other people who spend a lot of time in the sun can develop pterygium, a yellowish growth on the eye. Sunglasses can prevent these eye complications.
2. Don’t Wear Contacts While Swimming, and Use Goggles
Whether you’re swimming in a chlorine or saline swimming pool or a body of open water, bacteria and microorganisms will be with you. People who wear contact lenses should take them out before swimming because these irritants can get underneath the lens and may lead to infection.
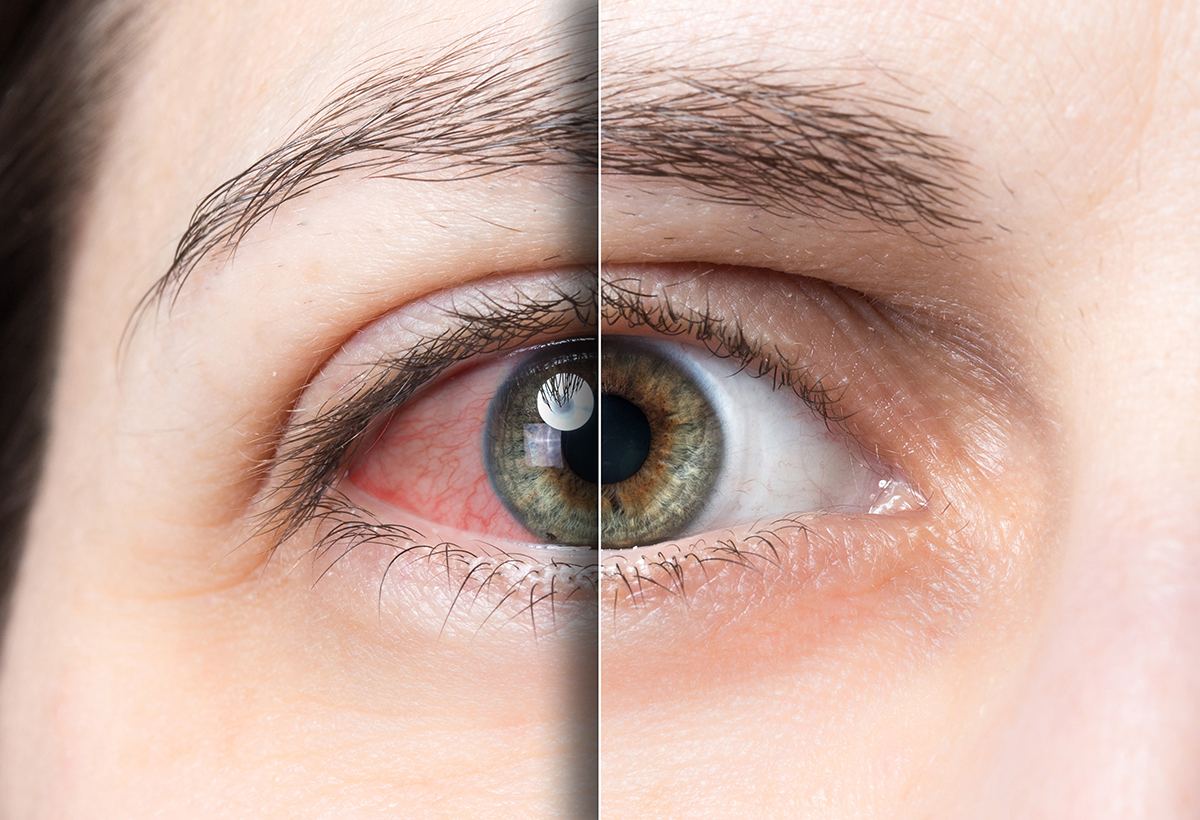
“Swimmer’s Eye” is another concern for people who spend much of their summer in the pool. Chemicals such as chlorine can alter the natural tear film and lead to temporary blurred vision, red eyes and a gritty feeling in the eyes — swim goggles and washing the eyes with fresh water can improve symptoms. Goggles also reduce the risk of contamination from bacteria in the water.
3. Protect Your Eyes from Dryness and Injury
The summer heat and dry environment may also affect the tear film and cause dry eye symptoms. Over-the-counter eye drops or artificial tears can help keep the eyes moisturized and refreshed. Wear protective eyewear that wraps around your eyes if you’re doing yard work or home improvement projects this summer. Mowing the lawn and trimming weeds can lead to eye injuries, as can construction work. More than half of all eye injuries take place in the home, but many can be prevented with proper eye care and protective eyewear.
Schedule an eye exam with our board-certified eye doctors at Wiles Eye Center by contacting our Kansas City, Missouri office at (816) 455-2020 or our St. Joseph, Missouri office at (816) 279-7015.
The post Summer Eye Care Tips to Lower Your Risk of Eye Diseases appeared first on .
from https://perfect2020.com/summer-eye-care-tips-to-lower-your-risk-of-eye-diseases/
via https://perfect2020.com


 Glaucoma is a group of diseases that cause damage to the optic nerve within the eye. The optic nerve is a bundle of over 1 million nerve fibers that are responsible for transmitting signals from your eyes to your brain. Did you know that Glaucoma is the leading cause of blindness across the entire planet? More than 60 million people worldwide are affected by this blinding condition. Nearly 3 million people in the United States alone suffer from Glaucoma. What’s even more shocking is that this number is expected to grow as years progress. The most detrimental fact about Glaucoma is that nearly half of those suffering from this condition are unaware that they even have it.
Glaucoma is a group of diseases that cause damage to the optic nerve within the eye. The optic nerve is a bundle of over 1 million nerve fibers that are responsible for transmitting signals from your eyes to your brain. Did you know that Glaucoma is the leading cause of blindness across the entire planet? More than 60 million people worldwide are affected by this blinding condition. Nearly 3 million people in the United States alone suffer from Glaucoma. What’s even more shocking is that this number is expected to grow as years progress. The most detrimental fact about Glaucoma is that nearly half of those suffering from this condition are unaware that they even have it.